Billing Optimization
Kick Your Billing Performance Into High Gear
With Features Like CCI Code Validation Edits
Clean claims are the cornerstone of your medical billing, and automated CCI Edits are how astute Billers achieve 99% first-pass claim acceptance. Leveraging the right tools can level-up your billing department’s performance to high gear, but billing at the highest level requires knowhow and the right software.
Top Billing Managers rely on embedded CCI Edits to ensure high first-pass claim acceptance rates.
Cleaner Claims & Faster Payments
Preparing clean insurance claims is already a complex and difficult task, but with features like PracticeSuite’s all-payer NCCI Edits that update continuously, your claims are validated prior to submission and your billing processes result in faster, more accurate claims and quicker payments, leveling-up your billing performance.
What is CCI Code Validation?
Accurate code validation with CCI edits helps prevent overpayments and underpayments, and speeds up your overall time to payment. It allows for better operational insight that helps your clinical, financial, and administrative areas work together more efficiently.
CCI code correction during charge capture helps eliminate the future need to hunt down rejection causes, contact payers, submit appeals, or monitor payer rules. Embedded CCI Edits ensure proper claim preparation and improve overall billing results.
What You'll Get

Expert support from experienced billers
What Coding Edits Do We Maintain?
CMS 1500 and UB04
Diagnosis Code Validation
Local Coverage Determination
National Coverage Determination
Gender & Age Edits
Advance Beneficiary Notice of Non-Coverage
Outpatient Code Edits
Medically Unlikely Edits
Correct Code Initiatives
CPT Edits
RVU Edits
Modifier Edits
Why are automated coding edits necessary?
CMS has over 14,000 edits in its National Correct Coding Initiative that update quarterly, whereas other payers may publish coding changes at any time. Only an automated correct-coding tool with real-time edits can insure accurate claims for quicker payments. PracticeSuite gives you the features and the tools you need to bill at the highest level.
At a Price You Can Afford
The AAPC puts it mildly: “Getting a clean claim out the door is not an easy process for any type of practice. The coding rules are diverse, and it takes a village to keep up with an ever-changing landscape. ..many policies and rules must be considered just to get an office encounter billed. In addition to evaluation and management services there are modifiers, procedure documentation, split shared, incident-to, diagnosis coding and many other factors that must be reviewed for correctness before billing any services.”
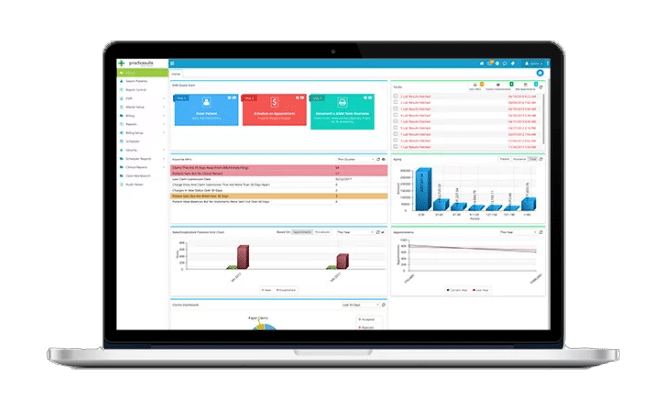
PracticeSuite offers high performance features that will take your RCM work to the next level
The revenue cycle is everything that affects payment before, during, and after the patient visit. Having the right tools helps get the job done right. Here are our top RCM performance features recommended to take your practice to the next level.
- CCI Edits: Clean claims are the cornerstone of billing efficiency.
- Batch Eligibility: know patient responsibility before the patient arrives.
- e-Payments: Take balances over the phone when patients call for an appointment.
- Scheduler: Reduce costly no-shows with reminders and online rescheduling.
- Reports. Reports. Reports: Track KPIs by role and department, 140 operational, billing and financial reports.
- Integrated EDI features: Clearinghouse features operate seamlessly within the billing software.
- Collections Manager: Work claims and denials with ease.
- e-Statements: Electronic statements are much faster, cheaper than paper, and patients prefer them.
Key Take Aways:
Clean claims form the foundation of an effective billing department, and automated CCI Edits are essential for achieving this goal. Utilizing the appropriate features can elevate your billing operations to peak performance.
Precise code validation minimizes the risk of overpayments and underpayments while accelerating the overall payment timeline.
Correcting codes during charge capture reduces the need for future follow-ups. Integrated CCI Edits guarantee proper claim preparation and enhance overall billing outcomes. The benefits are decreased denials and simplified denial management.
PracticeSuite equips you with the necessary features and tools to achieve high-level billing.
Check Out Our Blogs
PracticeSuite Announces Strategic Acquisition of MicroMD, Driving Rapid Growth and Enhanced Customer Experience
TAMPA, Fla., Sept. 16, 2025 (GLOBE NEWSWIRE) -- PracticeSuite, a leading provider of cloud-based practice management and revenue cycle solutions,...
Top 7 Revenue Cycle Management (RCM) Companies of 2025
Without the necessary cash flow, medical practices can’t properly care for their patients. That’s why, although the focus of healthcare...
AI Field Guide: What to Know Before Contract Renewal
So, you’re ready to explore the AI health technology landscape. We’ve got some checklists you can throw in your backpack,...
AI for Front Office
Imagine a front-office worker who doesn’t take vacations, happily texts patients about appointments instead of going to lunch, makes sure...
AI for Medical Billing
AI is the current sensation, and the hype is everywhere, but there is almost no academic research predicting its impact...
Risks and Rewards in AI for Clinical Documentation
EHRs were designed to improve patient care, but in so doing, they drastically increased physician workloads. AI promises to reverse...