AI is the current sensation, and the hype is everywhere, but there is almost no academic research predicting its impact on crucial areas of healthcare such as identity and access management (IAM), PHI, cybersecurity, HIPAA, or malpractice risk. This means we must rely on past technological experience to inform what early adopters can expect: a risky proposition for what will likely be remembered as a revolutionary leap for medicine, patient care, and medical practice management.
As a small practice needing robust technology and facing contract renewal, here’s what you need to know about AI to filter out the hype, avoid falling for technology that’s not ready for prime time, and make a well-informed purchase of practice management and medical billing software.
How AI Can Improve Your Back Office
There’s no question that today’s AI holds a great deal of allure for overworked doctors (i.e., all doctors) who are being promised help with charting, coding, and even clinical notes. Indeed, AI is poised to help providers in areas like decision support, clinical documentation, and being able to “talk” to an EHR:
But in this post, we’re focusing on the revenue side of the practice, where smart technology has already made some strides and has the potential to truly move the needle in revenue prediction, front- and back-office collections, and increasing efficiency of RCM teams and medical billing services laboring to maximize revenue for practices caught between shrinking reimbursements and escalating operational costs.
There are two main areas where AI can improve your practice’s back office: automation and enhancement. We’ll discuss each in this post, then offer advice for cutting through the AI hype when choosing RCM software.
AI Automation
AI has a huge role to play in automating repetitive tasks. These include data entry, eligibility verification, patient registration, updating patient information, providing real-time updates for patients (keeping them informed about bills and payments to reduce confusion), and payment posting.
The latter promises to eliminate the need for billers to post payments manually, a task they dread. Automated systems let your practice manager or head of RCM define the rules for electronic remittance advice (ERA) posting. The AI-driven software then automatically posts any ERA in the system according to those rules, which can be changed at any time.
Eligibility verification is another area of extreme interest to providers. AI has the potential to accelerate this process so that front-desk personnel and others can instantly see a patient’s coverage details, greatly reducing claim denials. Similarly, automated patient registration speeds up intake and can be tied into messaging aimed at decreasing no-shows.
AI Enhancement
As helpful as automation will be, AI’s ability to reduce billing errors, identify denial trends, streamline collections, and improve compliance with payer guidelines is where things get exciting. Importantly, this is all done using traditional AI (meaning it does a task using predefined rules and algorithms), not the more controversial generative AI.
Here are several capabilities you will find in advanced software:
- Find claims inconsistencies such as missing codes and duplicate entries
- Analyze denials to identify patterns that can be corrected
- Predict patient payment behavior to create personalized collection strategies
- Use advanced edit engines to facilitate more accurate charge capture and coding to comply with payer guidelines
- Smooth out cash flow with up-to-date patient statements
Caveat Emptor—Let The Buyer Beware
As scary as new technology can seem (i.e. “please, Hal, just open the pod bay doors”), the real fright for providers and practice managers around AI is less-than-true product claims around features that have not yet been released and/or proven out in a practice setting.
It’s unfortunate, but there are medical software companies claiming AI features that haven’t been thoroughly tested or simply don’t work. Similarly, in their rush to claim that their products are more intelligent than their competitors, not all companies selling AI features have put strong PHI security in place.
A lesser issue, but still concerning, is the general lack of evidence around AI in medicine. There is almost no academic research on which practice areas will benefit the most from AI.
Separating AI hype from genuine capabilities isn’t simple, but don’t let that stop you from asking questions of your billing software provider and any company pitching AI features to entice you. Remember that AI is still in its infancy, so claims that sound too good to be true might be just that.
RCM Software and AI
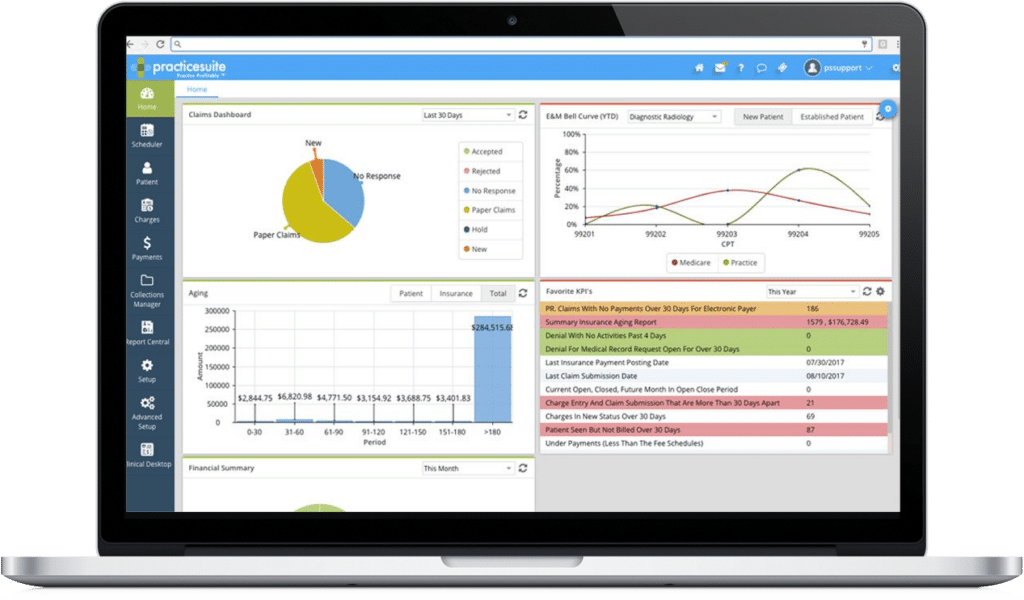
When it comes to RCM software, the most important thing is the flexibility of the underlying technology stack. This sounds geeky, but if a company offers fully cloud-based software and has already incorporated smart features such as ERA posting, automatic coding verification, and intelligent dashboards that can easily be customized, it’s more likely to successfully add AI features than a company using older, server-based technology.
As always, seek out vendors that provide for 100% HIPAA compliant, robust, end-to-end security with failsafe redundancy. Naturally, this should extend to any AI features or automation.
Finally, remain cognizant of AI’s limits. As amazing as this technology can be/will be, it cannot replace human interaction with patients. Understanding billing concerns, especially for those with complex medical conditions, will always require human intervention and empathy.
To learn more about PracticeSuite's approach to AI, visit our Artificial Intelligence page.