2019 Best Prior Authorization Solutions: HEI Global Health
In our prior authorization review of the best solutions for 2019, we’ve ranked seven vendors as the top options to help physician practices automate and speed up pre-authorization for their patients. Fifth on our list of top 7 prior authorization solutions for 2019 is HEI.
Here, we provide an in-depth review of our #4 choice HEI Global Health Prior Authorization Solution
Pros of HEI
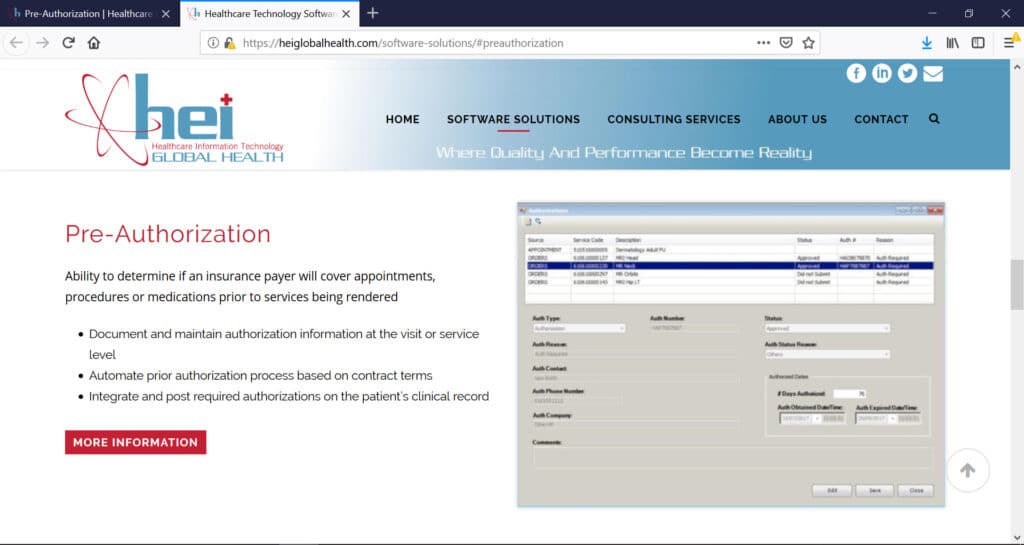
Authorizations can be worked manually or electronically based on individual insurance payer abilities, and can be flagged at the visit, scheduled appointment or individual procedure level. You can check pending authorizations and manually add authorizations to the work queue. When prior authorizations are pending, denied or require additional information prior to approval, these items are identified and can be worked out of an unauthorized work queue.
Authorization details such as status, number, reason, days-authorized, expired date, can be stored on each item that has been flagged. It can also document and maintain authorization information at the visit or service level; automate the process based on contract terms; and integrate and post required authorizations to the patient’s clinical record.
Cons of HEI Global Health Prior Authorization Solution
If there are any cons about the HEI application, it would be nice to have it work as an independent stand-alone pre-authorization module. But the benefit of the fully integrated health information system more than makes up for any downside.