2019 Best Prior Authorization Solutions: Azalea Health
In our prior authorization review of the best solutions for 2019, we’ve ranked seven vendors as the top options to help physician practices automate and speed up preauthorization for their patients. Third on our list of top 7 prior authorization solutions for 2019 is Azalea Health. Here, we provide an in-depth review of our #3 choice Azalea Health Pre-Authorization Services
Pros of Azalea
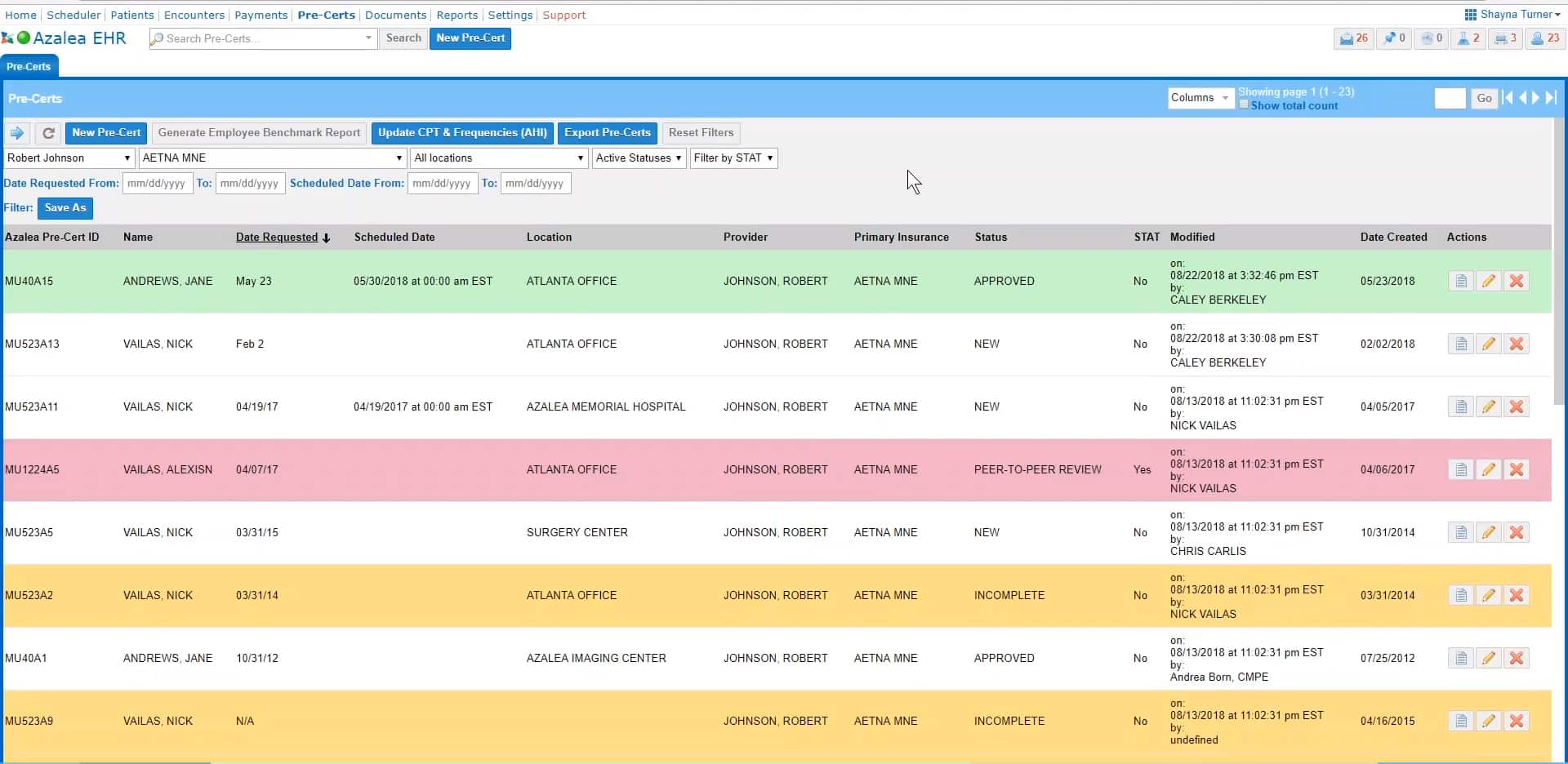
With prior authorization services from Azalea, you get an experienced partner owning the process to help maximize claim reimbursements with reliable and rapid turnaround, reduce duplication and data errors, and free up your people to focus more on your patients and less on paperwork. A secure, web-based portal allows for transparency and single-screen management, status-based filtering, procedure code look-up and more.
Azalea collects patient information from medical providers to obtain prior authorization for inpatient and outpatient procedures, in addition to precertification for hospital admissions.
Their experienced service staff uses a web portal interface to transmit patient data to appropriate areas within healthcare organizations. They work with physician offices and insurance payers, ensuring pre-certification and approval requirements for hospitals, outpatient facilities, and physician offices.
Cons of Azalea Health Prior Authorization Service
If there are any cons about the application, it would be for more payers to adopt electronic determination of benefits so that the process was streamlined for more plans and more patient scenarios. But more and more insurance payers are adopting EDI standards for electronic transactions.



